Intelligent agents for behavioural change
Identifying and modelling adaptive mechanisms
We all know about the benefits of a healthy and relaxed lifestyle, but achieving this in practice often remains a challenge. According to Dr Willem-Paul Brinkman of the Interactive Intelligence research group, intelligent systems can provide a solution. These so-called Behaviour Change Support Systems come in all shapes and sizes, such as mobile apps that offer people coaching to overcome their sleeping disorders, or virtual reality systems that allow sufferers of social phobias to practice with virtual characters, for example to help them get over their fear of giving presentations. These systems can also be used to teach skills such as negotiating or making decisions under pressure. During the past fifteen years, the Interactive Intelligence research group has focussed their research on mental health. Most people will be familiar with the research into virtual reality therapy systems. In a virtual environment, patients are exposed to situations that are frightening for them, and their fear decreases by virtue of habituation. In the early years the research focussed on the treatment of fear of heights or flying, but in recent years is has been expanded to include the treatment of social phobias and post-traumatic stress disorder (PTSD) among war veterans or people who were sexually abused in their youth. Another means of stimulating behavioural change involves using intelligent virtual health agents. These virtual coaches can provide information on a patient’s health and motivate them in the change process, but they can also help them to reflect on their goals and understand the progress they have made. These agents are often given human characteristics in order to trigger reactions similar to those produced by human coaches.
Stimuli
A key part of the research on systems like these involves identifying and modelling adaptive mechanisms that can be translated into a computer system. These systems must be able to observe the behaviour of the person; their perception, cognitions and emotions. This can be done indirectly with sensors, or directly by conducting a dialogue with the user. In addition, the system must be able to reason based on knowledge, and user and progress models. Finally, the system must also be able to respond, in order to steer the situation towards the intended objective. Often, the way to help the patient is through finding the right incentives or stimuli to change their behaviour. Since everybody is a little different, it is important to personalise such stimuli. ”You need to have a clear understanding of these people’s goals,” explains Willem-Paul Brinkman. “A system that understands what kind of individual it is dealing with can adapt its response to what it observes.”
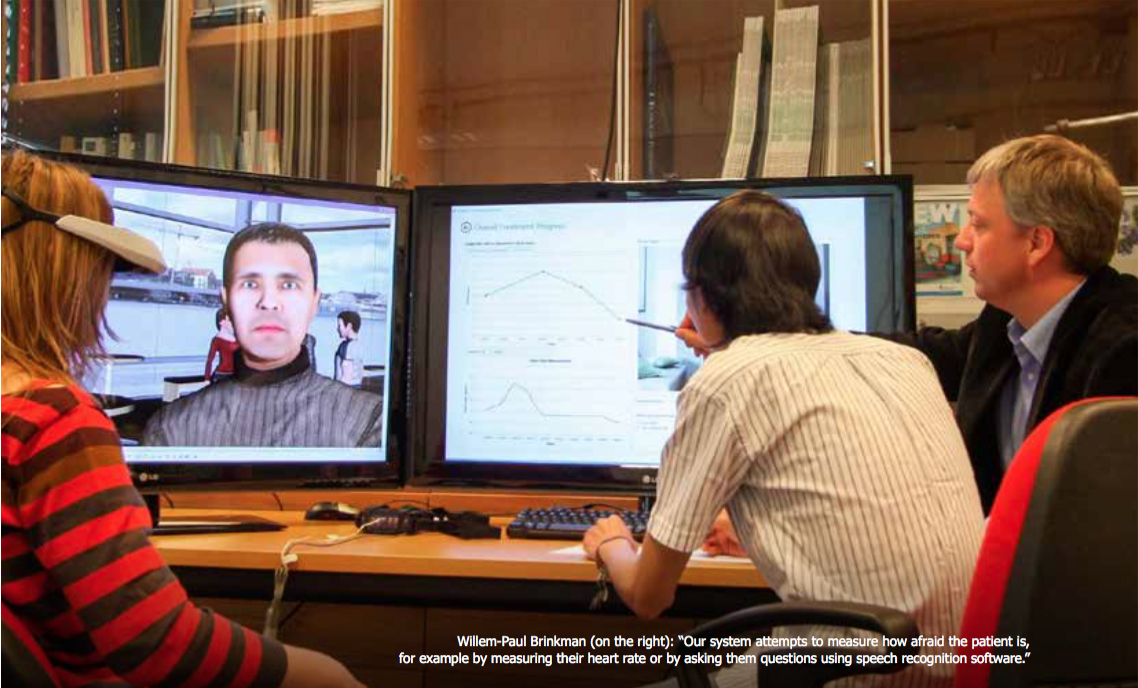
Room thermostat
Brinkman gives the negative feedback loop as an example of such a mechanism. He compares this mechanism with a room thermostat, which is activated when it gets cold and deactivated once the desired temperature has been reached. “The treatment of a social phobia requires creating a certain fear level: of you are not afraid you will not benefit from the experience of fear and if you are too afraid then the treatment will not work. Our system attempts to measure how afraid the patient is, for example by measuring their heart rate or by asking them questions using speech recognition software. If the system detects that the patient is not afraid enough, it will make the virtual experience dialogues more unnerving by asking more challenging questions or responding more negative to the patient’s answers. The system will continue to increase the pressure until it detects that the patient has reached the desired level of fear.”
Effect and acceptance
Testing the effectiveness and acceptance of the systems is an important part of the research. In order to ascertain whether the system has the desired effect, the TU Delft researchers collaborate with clinical partners. Together with the University of Amsterdam they conduct a study into computer-aided treatment of social phobias and with Erasmus University Rotterdam they examine such computer support in the treatment of PTSD. “Acceptance is crucial here: how do the patients experience it? What factors play a role?” Understanding this experience factor, involving aspects such as convenience, confidence and safety, tells the designers where they need to focus their efforts. Experiments are also being conducted in the faculty. These experiments serve as a preliminary trial to test whether the mechanism actually works. “For example, we are currently studying holiday memories. Can a virtual agent, with an ontology of events and a certain method of questioning, take the subject’s memories to a deeper level? If we can demonstrate that this is possible, then we will be ready for the next step: using a virtual agent to question PTSD patients about traumatic memories as part of their treatment.”
Advantages
According to Brinkman, a virtual health agent has clear advantages. “Sometimes it is easier to talk to a machine than to a flesh-and-blood person. Consider as an example PTSD patients with a sexual abuse trauma.” In addition, an agent always has time. And if the patient does not understand the agent it can repeat the routine as often as required. “Healthcare workers would like to be able to do the same, but it is simply not always practically feasible. This is an important social challenge for the future.” People today grow older than they used to and often suffer several chronic illnesses. The changing demography – reduction of the working population and ageing - means that there will be less people to provide this care in the future while more people will need it. “It would be ideal if certain cases could be dealt with by a computer, so that healthcare workers would have more time for those cases that require human interaction.”
Source: Katja Wijnands, Quadraat June 2015.